Douglas A. Nelson, MD, is double board-certified in medical oncology and hematology. He was a physician in the US Air Force and now practices at MD Anderson Cancer Center, where he is an associate professor.
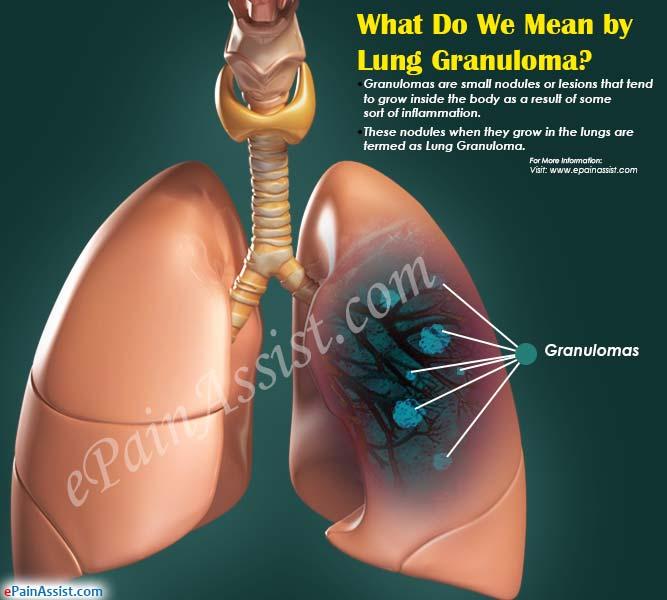
Learn about our Medical Review BoardTable of ContentsView AllTable of ContentsLung granulomas are common throughout the world, and can be challenging to diagnose. Rather than a specific disease, lung granulomas are areas of localized inflammation in the lungs that can be caused by a wide range of conditions. These range from infections, to autoimmune diseases, to environmental exposures, and more.
Frequently discovered as an "incidental" finding on an X-ray or computerized tomography (CT) scan, lung granulomas may not cause any symptoms. Other times, they may be associated with respiratory symptoms (such as a cough) or symptoms related to the underlying condition that is responsible for the granuloma or granulomas. The diagnosis usually requires a combination of a careful history, imaging tests, laboratory tests, and often a biopsy. The treatment will depend on the underlying cause.
Lung granulomas may also be referred to as "granulomatous lung disease."
Lung granulomas are often first noted as a lung nodule or multiple pulmonary nodules on a chest X-ray or chest CT scan. As they can sometimes mimic lung cancer on a scan, they frequently cause considerable anxiety when discovered.
Lung granulomas are localized (focal) areas of inflammation in the lungs. There may be a single granuloma, or multiple granulomas scattered throughout the lungs.
A lung granuloma is a localized collection of inflammatory cells.
The commonality among granulomas is that they occur as a "normal" bodily process in which the body attempts to contain something foreign in the lungs. In other words, a granuloma is essentially an area of microscopic quarantine in the lungs. The foreign material may be a microorganism (such as a fungus or bacteria), pieces of talc or metal, or products related to an autoimmune reaction in the body.
Under the microscope, a granuloma is comprised of inflammatory cells called activated macrophages (epithelioid histiocytes). Other cells, such as lymphocytes and Langerhan's giant cells may also be found.
Granulomas may be present only in the lungs, but depending on the cause may occur in other areas of the body as well, such as the skin and lymph nodes.
Lung Granuloma Symptoms
The signs and symptoms of lung granulomas may range from no symptoms at all to widespread symptoms related to the underlying cause of the granuloma or granulomas.
Many lung granulomas are detected "accidentally," when a CT scan of the chest is done for another reason or during lung cancer screening. When this occurs, it is sometimes difficult to know whether the granuloma is associated with the reason for testing or simply an incidental finding (something referred to as a "red herring" in medicine).
Many granulomas do not cause any respiratory symptoms. Exceptions may occur, however, if the granulomas lie near the large airways of the lung or if they are a lot of granulomas present. In addition, granulomatous lung disease may be associated with other lung diseases (such as interstitial pneumonia) that cause symptoms.
When present, symptoms may include a cough, wheezing, shortness of breath, or repeated respiratory infections.
When symptoms are present, they are frequently related to the underlying cause of the granuloma.
For example:
When considering the underlying causes of a granuloma, it's important for people to talk to their healthcare provider about any symptoms they are experiencing, including vague symptoms such as fatigue.
Causes
Learning that you have a lung granuloma can be frightening, and many people worry that an abnormal spot on a chest X-ray or CT could be cancer. Fortunately, most lung granulomas are benign (not cancerous). While there are many potential causes, fungal infections and tuberculosis are most common overall.
A granuloma is actually caused by the body's response to an offender. This inflammatory response occurs as the body tries to "wall off" a foreign substance, whether it is an infectious organism, materials such as talc or some metals that find their way into the lungs, or immune complexes related to autoimmune conditions. As such, a granuloma isn't "abnormal" itself but is a sign of something else happening in the lungs.
Granulomas can be described as "necrotizing granulomas," meaning that there is an area of necrosis (cell death) within the granuloma, or non-necrotizing. Necrotizing granulomas are more common with underlying infections.
Possible causes of a granuloma or granulomas can be broken down into a few main categories.
Infections are the most common cause of granulomas, and include:
Tuberculosis: Worldwide, tuberculosis is the most common cause of pulmonary granulomas, though the incidence has been increasing recently in the United States.
Non-tuberculous mycobacteria: Mycobacterial infections such as Mycobacterium avium complex and Mycobacterium kansasii are an important cause.
Fungi: There are more than 140 types of fungal infections that can lead to lung granulomas, the most common being:
Parasites: Parasitic infections as a cause are less common in the United States, but may still occur.
Bacterial: Bacterial infections (other than those associated with aspiration) are less common causes.
Inflammatory granulomas are often associated with underlying symptoms related to the disease.
Sarcoidosis: Sarcoidosis is an inflammatory disease that can affect many regions of the body, and often begins with swollen glands, skin changes, fatigue, and joint pain and swelling.
Necrotizing sarcoid granulomatosis: Considered a separate condition from sarcoid by many, the condition may be erroneously diagnosed as tuberculosis.
Bronchocentric granulomatosis: This an inflammatory condition that involves the bronchioles, and is thought to be a response to some type of injury to the lungs.
Inflammatory bowel disease: With inflammatory bowel disease (such a Crohn's disease and ulcerative colitis), granulomas may occur not only in the gastrointestinal tract, but other regions of the body such as the lungs. In one study, 21% to 36% of people had evidence of these granulomas outside of the GI tract.
Several of the drugs used to treat inflammatory bowel disease have also been associated with the development of lung granulomas (see below).
There are a number of different environmental exposures that may lead to pulmonary granulomas.
Hypersensitivity pneumonitis: Hypersensitivity pneumonitis, or inflammation of the lungs due to an allergic reaction, may occur with a number of different exposures. Some of these include fungi (such as Penicillium and Aspergillus), bird proteins, and chemicals such as some dyes.
Hot tub lung: Hot tub lung may occur in people who use hot tubs, and is caused by Mycobacterium avium complex.
Berylliosis: Exposure to beryllium (usually on-the-job) may result in berylliosis.
Other metal dust exposures: A number of other metal dust exposures may result in symptoms similar to berylliosis. Some of these include aluminum, titanium, zirconium, cobalt, and silica.
It's now thought that silica may actually be the trigger for necrotizing sarcoid granulomatosis noted above.
Talc granulomatosis ("drug abuser's lung"): Talc (hydrated magnesium silicate) granulomas are most often related to illicit drug use. It is seen primarily with the injection of crushed up pills (hence, the talc) such as opiates, barbiturates, and methylphenidate.
Rarely, the inhalation of cosmetic talc (talc in personal care products) may lead to talc granulomas, though fewer than 10 cases have been reported.
Medications: Adverse reactions to a number of different medications have been associated with the development of lung granulomas. This can be confusing, as some of these drugs are used to treat medical conditions that are associated with pulmonary granulomas. Some of these include:
Lung granulomas may occur in a number of different autoimmune conditions.
Rheumatoid arthritis: Lung granulomas (necrotizing granulomas) are relatively common in people with rheumatoid arthritis, and may occur in the lungs as well as under the skin (subcutaneous). They may occur related to the underlying disease, or as an adverse reaction to medications used to treat the disease.
Sjogren's disease: A number of lung diseases including lung granulomas are associated with Sjogren's disease.
Vasculitis: Vasculitis is a term that refers to chronic inflammation of blood vessels, and may occur in blood vessels anywhere in the body. The most common sites, however, are the lungs and kidneys. Types of vasculitis associated with granulomas include:
Immunodeficiency may be associated with granulomas in adults or children.
Granulomatous–lymphocytic interstitial lung disease: Granulomas may occur in association with common variable immunodeficiency in adults or children, and it's thought that these syndromes are underdiagnosed. The condition is relatively common, and most often diagnosed in people in their 20s or 30s.
Recurrent Respiratory Infections in AdultsGranulomas are usually associated with benign conditions, but may sometimes be seen with cancer:
Other conditions in which lung granulomas may occur include pulmonary Langerhans cell histiocytosis/eosinophilic granulomatosis (PLCH). This is an uncommon condition that is usually seen in young adults who smoke. The cause is unknown.
Diagnosis
Due to the wide range of potential causes, diagnosing lung granulomas can be challenging. In addition to a careful history and physical examination, lab tests, imaging tests (such as chest CT), pulmonary function testing, and most often, a lung biopsy, are needed.
The diagnosis of a granuloma begins with a careful history of symptoms, including those that seem unrelated to the lungs. When symptoms are present, it's important to note whether these are of recent onset (acute) or have been ongoing for some time (chronic). Where a person lives may be helpful in narrowing down possible fungal causes, and a history of travel may raise the likelihood of tuberculosis. On the job exposures (such as to beryllium) should also be noted.
A history of repeated infections (such as sinusitis) may be noted in people who have immunodeficiency. As immunodeficiency syndromes as a cause of repeated infections are underdiagnosed in both adults and children, and it's important to let your healthcare provider know if you've had repeated sinus or other respiratory tract infections.
Recurrent Respiratory Infections in ChildrenA lung granuloma or granulomas are often first noted "by accident" when a chest X-ray or chest CT scan is done for another reason. A high-resolution chest CT scan is a very important step in the diagnosis and evaluation of a lung granuloma as calcium deposits in granulomas often make them visible. For people who have a lower resolution CT scan, such as those done for lung cancer screening, a high-resolution scan should be done. In some cases, a chest MRI may be helpful.
A PET scan is often done if there is concern about cancer, vasculitis, and inflammatory diseases, though the rate of false positives (a scan that is suspicious for cancer but is not cancer) is high.
It's important to note that, in people who have diabetes, small lung granulomas are often misdiagnosed on PET as being lung cancer.
PET scans can be helpful in the diagnosis, but in people who have diabetes, pulmonary granulomas are sometimes misdiagnosed as being cancer.
When evaluating possible lung granulomas, radiologists look at a number of characteristics that may help narrow down the potential causes. Some of these include:
A number of laboratory tests can help with determining the causes of lung granulomas.
CBC: A complete blood count (CBC) can sometimes be helpful. For example, an increased number of the type of white blood cells called eosinophils (eosinophilia) may be seen with parasitic infections or with allergic bronchopulmonary aspergillosis.
Causes of EosinophiliaSerology: Diagnosing fungal infections as a cause of lung granulomas is primarily done via serology tests (blood tests), rather than tests that isolate the fungi (although fungi may be seen on a microscope slide after a biopsy).
TB testing: Testing for tuberculosis is important for anyone who has a lung granuloma of unknown cause whether they've traveled or not. A skin test or blood test may be done, as well as cultures.
How Tuberculosis is DiagnosedTesting for non-tuberculous mycobacteria: A culture and/or PCR for atypical mycobacteria may be considered.
Immunoglobulins: Serum IgE and IgE may be increased when Aspergillus is responsible for a granuloma.
A bronchoscopy is often done as a way to visualize the airways, and to sometimes perform further tests such as bronchoalveolar lavage or an endobronchial ultrasound/biopsy. In a bronchoscopy, a flexible tube is inserted (following sedation) through the mouth and threaded down to the large airways of the lungs.
Endobronchial ultrasound: An ultrasound probe may be attached to a bronchoscope to allow physicians to visualize regions in the lungs near the airways. With special tools, a biopsy may be done (transbronchial biopsy) for granulomas located near the airways.
Bronchoalveolar lavage: Bronchoalveolar lavage is a procedure done during a bronchoscopy, and is thought to be a very sensitive method for detecting hypersensitivity pneumonitis as a cause of granulomas. During the procedure, sterile saline is injected into the lungs through the bronchoscope and then suctioned out. The sample obtained contains cells from the lower respiratory tract that can then be examined under the microscope.
Very often, a biopsy specimen is necessary to determine or confirm the precise cause of a lung granuloma.
A lung biopsy specimen may be obtained in a few ways:
Evaluation of a biopsy sample involves looking at the cells under the microscope, as well as special stains such as the Grocott methenamine silver (GMS) stain for fungi, the Ziehl-Neelson stain for mycobacteria, and others.
Under the microscope, some fungi may be visualized. With aspiration, material such as vegetable matter may be seen. If necrosis is seen, it suggests some causes more than others (such as infection). Other substances, such as talc may also be seen.
Other tests may be performed depending on the suspected underlying cause of a granuloma. If multiple granulomas are present, or if other lung diseases are present along with a granuloma, pulmonary function testing will likely be recommended as well.
Treatment
The treatment of lung granulomas will depend on the underlying cause. In general, most granulomas do not need to be surgically removed. Exceptions may occur if the granuloma or granulomas are causing symptoms or if the diagnosis is uncertain.
Some potential treatments include:
Lung granulomas are common (and the incidence will likely increase with the broader use of lung cancer screening), but since there are many potential causes it may take some time to diagnose. This can be frustrating and anxiety-provoking at the same time.
Regardless of the potential cause, it's important to be your own advocate in your health care and to ask a lot of questions. Sometimes, getting a second opinion is wise; both for any symptoms you have and the findings on a scan, but a second opinion on your pathology report if you had a biopsy as well. Reading biopsy slides of granulomas is complicated, and having a pathologist who specializes in reading these slides may be needed.
Was this page helpful?Thanks for your feedback!Limiting processed foods and red meats can help ward off cancer risk. These recipes focus on antioxidant-rich foods to better protect you and your loved ones. Sign up and get your guide!
You're in!Thank you, {{form.email}}, for signing up.
There was an error. Please try again.









